PTSD


Post-Traumatic Stress Disorder
Participation in traumatic events can lead to PTSD (Post-Traumatic Stress Disorder) and related symptoms that make it difficult to live your life. Examples of events that can trigger PTSD include wars, crimes, fires, accidents, the death of a loved one, or abuse of some form.
PTSD symptoms are generally grouped into four types: intrusive memories, avoidance, negative changes in thinking and mood, and changes in physical and emotional reactions. Symptoms may include nightmares or unwanted memories of the trauma, avoidance of situations that bring back memories of the trauma, heightened reactions, anxiety, or depressed mood.
Treatment includes different types of trauma-focused psychotherapy as well as medications to manage symptoms. At Overland, we have the tools we need to identify and help patients overcome PTSD. The PHP and IOP services at Overland utilize an evidence-based approach. It addresses both short-term and long-term consequences of violent victimization and neglect, including mental health symptoms, such as posttraumatic stress disorder (PTSD), depression, and substance abuse.
PTSD: IOP Treatment
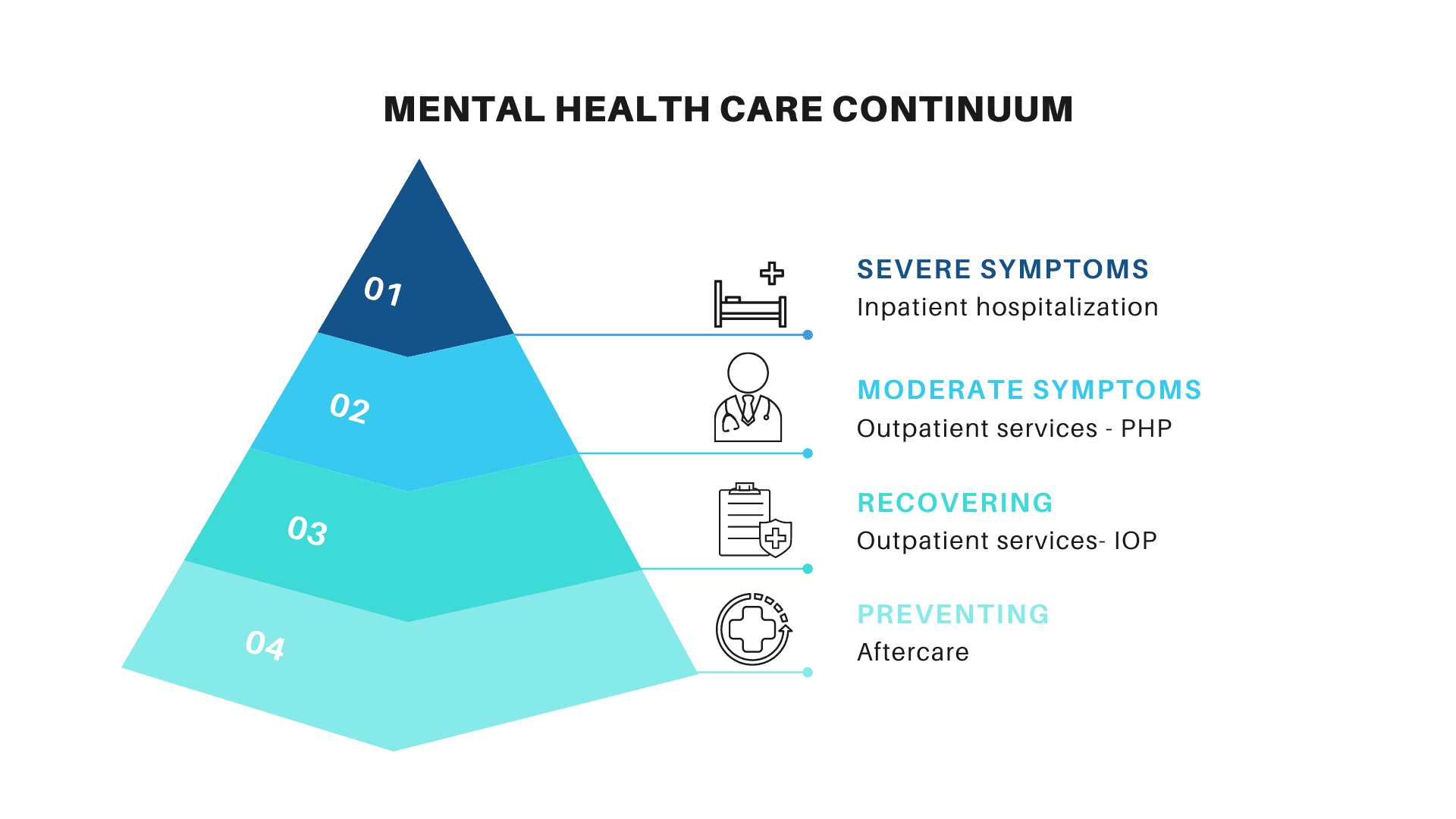
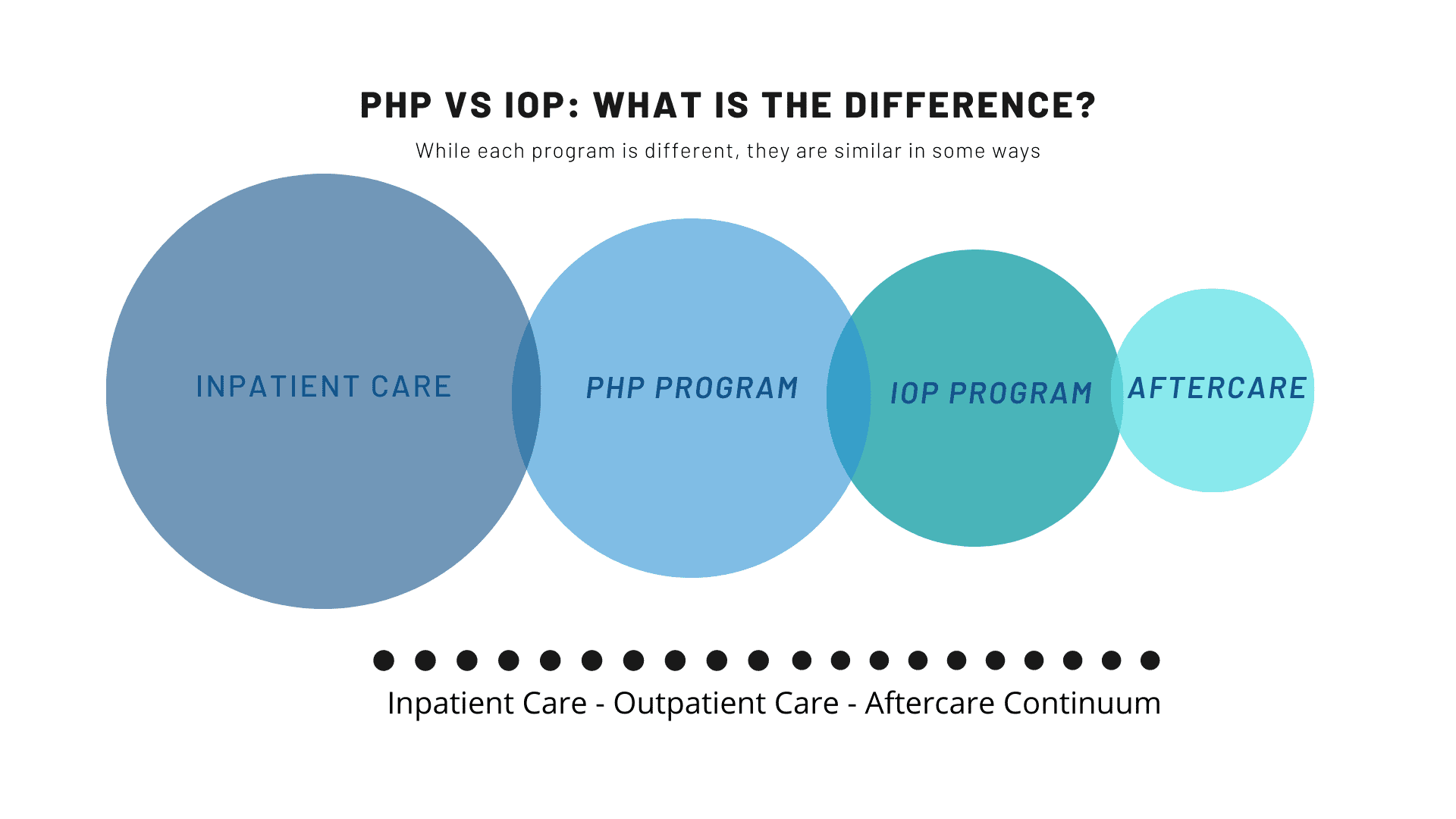
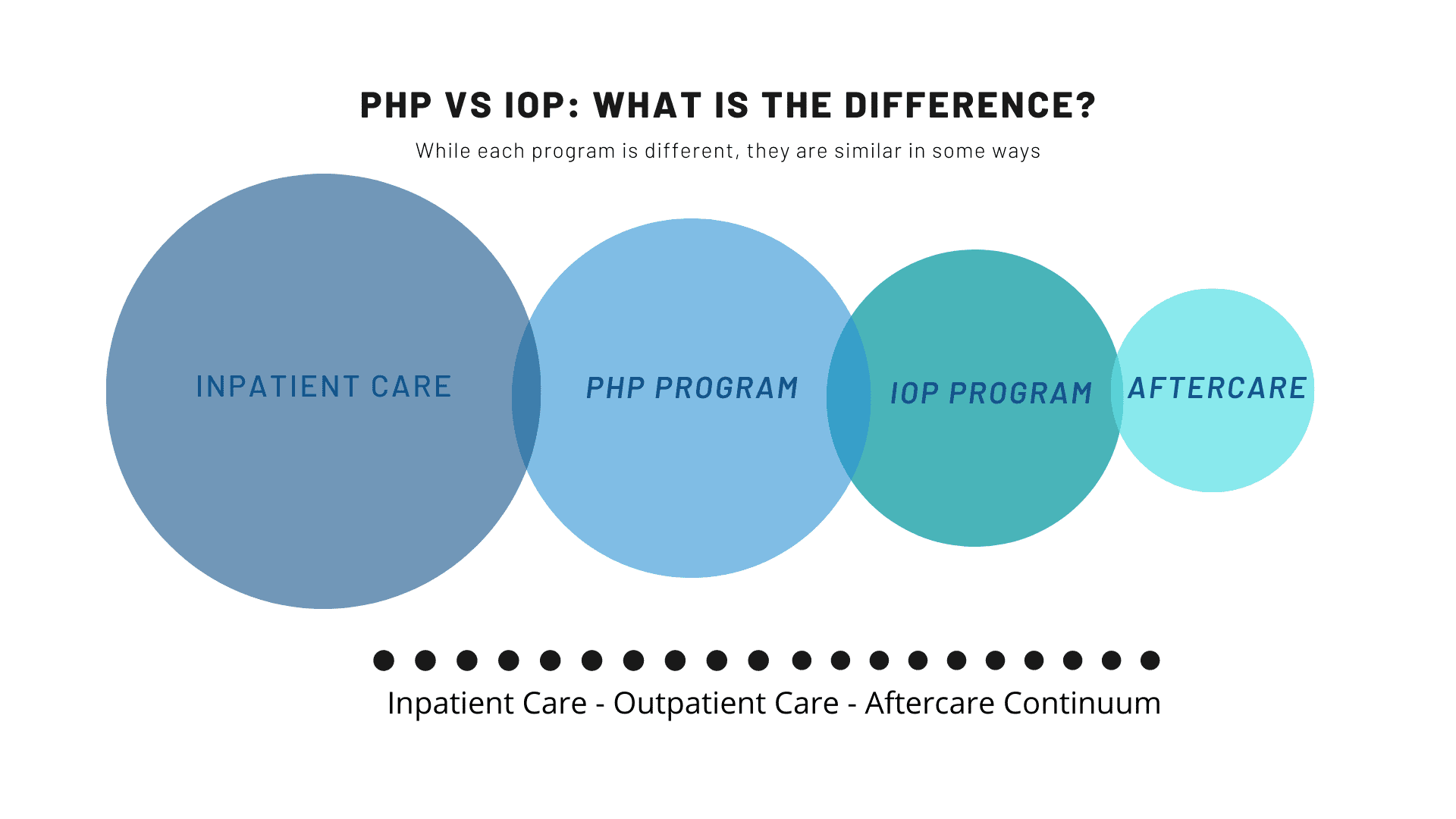
IOP programs are meant for people who do not require inpatient treatment and have moderate to mild symptoms. Therefore IOP programs are mostly recommended as a subsequent stage for patients who have left the inpatient facility or are stepping down from the more intensive PHP given that the symptoms identified and monitored are under control, implying that you might only require a support structure. IOP allows you to adhere to your treatment program after regaining the confidence to begin a new sober life with just the right amount of support. Many IOP –affiliate programs encourage participants to engage in a 12-step program to help streamline their path to sobriety. Your insurance cover limits also play a vital role in determining the extent of IOP. IOP programs usually last approximately 3-4 hours per day, 3-5 days a week.
PTSD: PHP Treatment
Patients tend to enter into PHP after completing their detoxification or inpatient treatment directly. In most cases, PHP requires the patient to be available for treatment daily. The main difference is that more of the patient’s time is required each day than the IOP. PHP programs usually last about 5-6 hours per day, 3-5 days per week.
PHP programs have significant amounts of individual and group therapy. They are taught better coping mechanisms to deal with their stress as alternatives to turning to alcohol and drug abuse for solace or self-medication. PHP is sometimes referred to as day- treatment to capture the idea that a patient will be receiving care on a nearly full-time basis during the day and allowed to go home in the evenings.
What Is Post-Traumatic Stress Disorder (PTSD) ?
Post-Traumatic Stress Disorder (PTSD) can manifest in a wide variety of ways. Typically, PTSD develops after an event or series of events that are particularly traumatic or make a person feel helpless. Participation in stressful circumstances over which you have no control, such as a car accident, war, or being the victim of a crime or abuse—whether physical, sexual, or emotional—can all be potential sources of trauma.
How Can Overland IOP and PHP Help With Post-Traumatic Stress Disorder (PTSD)?
At Overland IOP, we have seen PTSD that results in persistent stress, depression, anxiety, chronic pain, sleep disorders, and feelings of hopelessness and shame that can interfere with your daily activities. We have a wide variety of therapies and techniques we can use to identify and help you to overcome PTSD including dialectical behavior therapy, cognitive behavioral therapy, EMDR, mindfulness, hypnotherapy, and psychotherapy.
Services
Although some addicts do recognize the problems their addiction has created and seek treatment and recovery on their own, this is not the case with everyone.
TREATMENT COVERED BY YOUR INSURANCE
Call today for same-day insurance approval & admissions!
Recovery Starts Today!
Mental Health Focus
We focus on mental health & co-occurring disorders treatments


Mental Health Focus
We focus on co-occurring disorders and mental health treatments
Individualized Care
We deliver a high level of individualized care
Experienced & Compassion Staff
We have over one hundred years of cumulative experience & a high success rate
Tracks All Day
Our IOP and PHP programs offer morning, afternoon, or evening options.
Case Management
We provide evidence-based case management
Safe Environment
Enjoy safe environment where you can focus on recovery & healthy lifestyle
Insurances Accepted
We accept most private & corporate insurances
Supportive community
We offer options to connect with people at all stages of recovery
Verified Testimonials
From Patients Who Wanted To Share Their Statement & Info.


Joel Herrera Los Angeles
This is a great program, the treatment team was great and really helped me to learn to curb my cravings and reduce behaviors that I didn’t even realize had been harming me


Jeremy California
Overland IOP completely helped me to recover from many anxieties and depressive thoughts I had prior to attending treatment here. They provided me with the tools to move on and live life on life’s terms. Therapist, group facilitators, case workers are very professional. I would recommend this place to anyone with addiction and/or mental health issues. I owe my newfound freedom and happiness to this place and it’s wonderful staff!


Hakeem Yousef Los Angeles
Very satisfied with my experience! Overland offered me the support that I needed to overcome my mental health obstacles. My therapist was extremely helpful, supportive, and always knew when to ask the right questions. The sessions I had with my therapist helped me address underlying factors in order to go about achieving stability in a constructive fashion. After visiting, I can say that I have much more direction and understanding when dealing with adverse scenarios than before. thanks so much!


Janet Dade LA
Overland IOP saved me from an unhealthy relationship!!! It saved my life! The staff is all so friendly and helpful! I’ve never been to an IOP like this. Thanks to Andy , Gracie , Eden, and the rest of the staff for being so helpful and supportive and to my fellow group members!


Madie Pino Los Angeles
Great therapists, super helpful staff. This place helped me with my recovery and also personal life issues


Jessica Armstrong
I had a life-changing experience at Overland. Staff was phenomenal. I’d highly recommend to anyone struggling.


Trevor Hahn LA
Overland was a great experience. I really appreciate the staff and sense of community that was created there. I made lifelong friends that are there for me no matter what and that will help me continue this journey of recovery. The groups are helpful and helped me gain great insight into myself and my addiction. I’m super grateful I was able to find a treatment center that cared so much about me as an individual.


John Moriarty NJ
Quality IOP with a true mental health track. I have referred many clients here. New management and ownership are top notch. Andrew and his team show they care about their clients recovery and growth.